Improving the Nutritional Intake and Physical Activity of Children from Low-Income Households via Family, School, and Workplace Policy
Download Policy Brief (PDF)
Download Executive Summary (PDF)
Talking Points
- Childhood obesity remains high in racially and ethnically diverse low-income families.
- By 2030, 16%–18% of all health care costs in the United States will be obesity related.
- Factors in the home environment have shown promising results in addressing childhood obesity; as a result, similar strategies could be implemented in other environments.
- Nutrition, physical activity, and family meals can be integrated into existing workplace and school intervention programs.
- The entire family can be included in interventions that take place outside the workplace and schools to reduce childhood obesity.
Abstract
Childhood obesity remains high, especially among children from racially and ethnically diverse and low-income households, and it is associated with numerous negative health consequences in adulthood. Family, home, school, and workplace environments are recommended areas for expanding policies and implementing strategic interventions for child obesity designed to improve nutritional intake and increase physical activity. Family-based interventions offer a variety of strategies to lower the incidence of obesity. Programs such as the federally funded Child and Adult Care Food Program can be extended to work with families and caregivers in schools. Further workplace wellness programs could use federal programs such as the USDA Expanded Food and Nutrition Education Program to establish policies and initiatives that extend obesity interventions to employees’ families.
Child and Family Obesity and Health
Childhood obesity prevalence has reached epidemic status in the United States. It is associated with a predisposition for adulthood obesity and with negative health, interpersonal, and economic outcomes that endure throughout an individual’s life span. Childhood obesity is associated with adolescent and adulthood obesity, the risk of chronic diseases (including type 2 diabetes and metabolic syndrome), functional limitations, depression and poor self-esteem, and premature adult mortality.1 Obesity is also associated with children’s lower academic performance, increased behavioral problems, and increased likelihood of being bullied.1 Furthermore, individuals with obesity incur higher health care expenditures than those of normal weight.2 It is estimated that obesity-related health care costs will reach between $860 billion and $957 billion by 2030, which equates to 16%–18% of total health care costs incurred by all Americans in the health care system.3 These negative health and economic outcomes associated with obesity necessitate prevention-based research as well as program and policy interventions.
Many home-based efforts to reduce childhood obesity have shown promise, yet childhood obesity prevalence continues to increase, especially in children from low-income and racially and ethnically diverse households. Extending the successful elements of existing interventions to other environments that also influence familial interaction, such as school and work, may produce more dramatic effects on reducing the prevalence of childhood obesity. Within both environments, policies and practices exist that, if extended and expanded, could apply family-inclusive intervention strategies to increase children’s diet quality and physical activity.
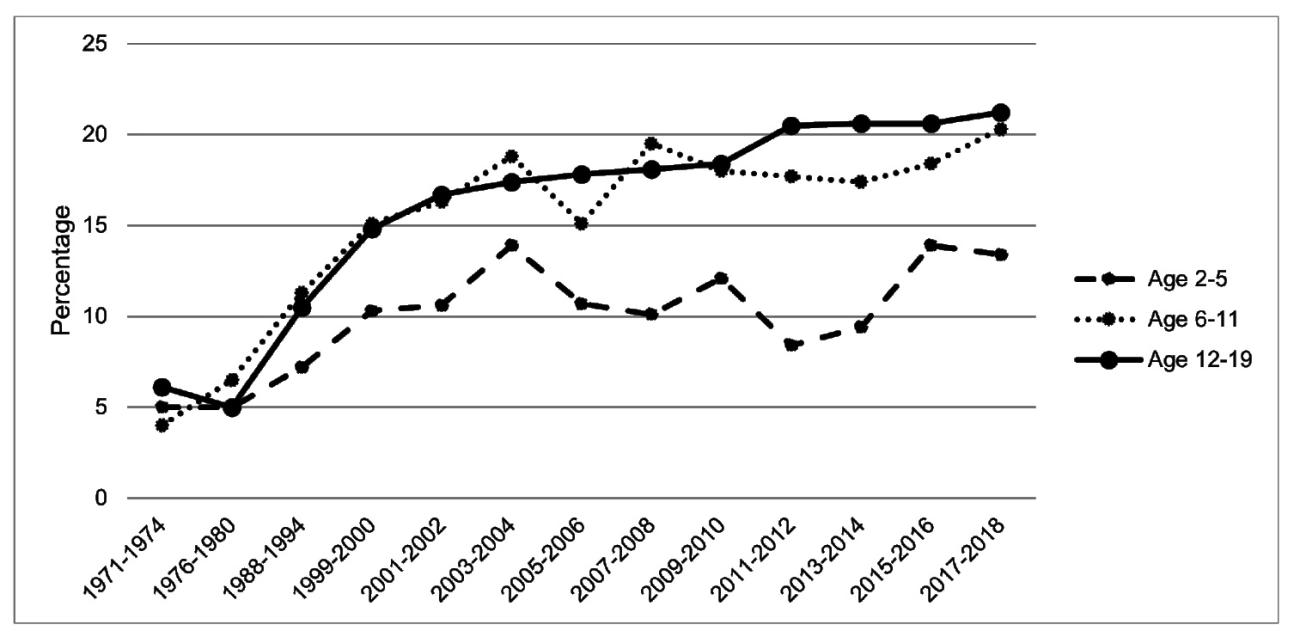
Childhood Obesity Trends
Since 1980, national childhood and adolescent obesity prevalence has increased and continues to rise (Figure 1). Among racial and ethnic minorities (e.g., Black and Hispanic children and adolescents) and children from lower socioeconomic status (SES) households, obesity is becoming increasingly prevalent.⁴ Since 1988, obesity rates have been higher among Hispanic boys and non-Hispanic Black girls than they are among non-Hispanic White boys and girls.⁵ According to 2017–2018 data, 25.6% of Hispanic and 24.2% of Black children and adolescents aged 2–19 years were obese (compared to 16.1% of White children and adolescents).⁵
SES and Child Obesity
During 2011–2014, obesity prevalence among children and adolescents aged 2–19 years with household income of less than 130% of the federal poverty level was 18.9%; further, the obesity prevalence rate was 21.6% among children and adolescents whose parent had an educational attainment of high school or less.⁶ Among children aged 10–17 living in low income, low education, and high unemployment households, obesity prevalence increased from 23% to 33% from 2003 to 2007.⁷ A systematic literature review published in 2017 showed the strongest correlations between rapid growth during the first 2 years of life (i.e., large weight difference between two time points during infancy) and later obesity among children of racial and ethnic minorities.⁸ Children from low-income households are at a 3.4–4.3 times greater risk of becoming obese than for their higher-household-income counterparts.⁷ The divergence in obesity prevalence associated with income demonstrates the need to dedicate obesity intervention efforts to children from low-income households. Thus, the following recommendations and strategies are intended to address obesity prevalence specifically among children from low-income households.
Avenues to Address Childhood Obesity
Primary strategies for reducing obesity among children from low-income households focus on bolstering the nutritional value of food intake and increasing physical activity levels. Interventions focus on these areas because they address two main causes of obesity: increased consumption of energy-dense, nutrient-poor foods and increasingly sedentary lifestyles.9,10 Research examining the association between calorie density and weight gain has called for enhancements in the “healthfulness” of food-related infrastructure to reduce obesity prevalence.11 Therefore, efforts to substitute energy-dense foods with more nutritious options lower calorie-density ratios and act in opposition to obesity-causing overconsumption of calories. Children from low-income households are especially vulnerable to consuming energy-dense, nutrient-poor foods, as these foods are most affordable and abundant in neighborhoods classified as low income.⁹
Family meals have been linked with healthier diet quality among children, including greater intake of fruits, vegetables, and grains and lower intake of sugar-sweetened beverages.12,13 In addition, frequent family meals are associated with fewer unhealthy weight-control practices or disordered eating behaviors,14 and are associated with reduced risk of overweight and obesity.14-16 In general, children from low-income households have less frequent family meals than children from higher-income households.13 Interventions to improve the frequency of family meals among lower-SES families have shown improvements in children’s weight.17 These compelling research findings suggest that improving the frequency of family meals is a way to improve nutritional status and reduce obesity risk among lower-SES families.
Encouraging physical activity in children augments the positive effects of enhanced nutrition and is crucial to healthy development. It is recommended that children aged 6–17 years participate in moderate to vigorous physical activity for at least 1 hour daily to meet standards set by the U.S. Department of Health and Human Services.18 Physical activity has been shown to reduce risk factors of metabolic disease and weight gain and to enhance factors that protect and promote healthy lifestyles.10 Physical activity increases caloric expenditure, offsetting the effects of caloric overconsumption and protecting against weight gain.19 Living in a lower-income household is associated with less physical activity among children.20 Thus, creating opportunities to encourage and integrate physical activity among children and adolescents from low-income households could counteract the rising prevalence of obesity among this population and is an important component of obesity interventions.
Policies identified in the following sections focus on improving nutrition, promoting family meals, and increasing physical activity among children from low-income households. All policy extensions and recommended initiatives enumerated in this brief are listed in Table 1.
Family and Home-Based Interventions
Family-based therapy (FBT) and interventions are designed to reduce childhood obesity through various strategies (e.g., improving nutrition and dietary intake, increasing physical activity levels, limiting sedentary activity).21,22 These programs significantly reduced weight in overweight or obese children and parents.22,23 Parental weight loss is associated with greater success in reducing obesity among children, as parents can influence child weight outcomes by modeling healthy behaviors and making changes in the home environment.21 The family-inclusive nature of FBT programs has produced more enduring weight reductions in children than programs that treat children or parents in isolation.21,22 Therefore, including parents in intervention strategies increases the potential to yield long-lasting outcomes among children from low-income households.
Children and families of racially and ethnically minoritized households and from poor and single-parent households show greater attrition in obesity prevention and intervention programs, which may explain the increase in obesity among these groups despite the effectiveness of FBT programs.24 Some common reasons for attrition include costs involved (e.g., health insurance does not cover program costs), conflicting schedules (e.g., school, work), and the program not meeting their expectations. Because interactions with family members, peers, and teachers influence children’s behaviors,25 extending FBT-based programs to other environments that influence children and families, such as school and work, could contribute to reducing attrition and increasing successful outcomes from FBT interventions.
Opportunities in Schools
Improving the nutritional quality of food served and sold at schools and increasing physical activity are both important to enhancing nutrition and health among children living in low-income households. School-based policies and interventions that focus on improving nutrition and encouraging physical activity have shown promising results in reducing childhood obesity.26-28
Under the Healthy Hunger-Free Kids Act of 2010 (HHFKA), schools that participate in the National School Lunch Program and the School Breakfast Program were required to align their meals with the 2010 Dietary Guidelines for Americans, including increased servings of fruits, vegetables, and whole grains; reduced levels of sodium and saturated fat; and the serving of fat-free or low-fat milk.29 After implementing HHFKA, the school nutrition environment improved, and the average calorie intake for children was reduced27 and more fruits and vegetables were consumed. Increasing the nutritional quality of school menus under the HHFKA is comparable to strategies implemented in community-based obesity prevention programs (e.g., Go for Health; Coordinated Approach to Child Health, or CATCH; New Zealand’s APPLE project26,30) that resulted in significant reductions in child calorie and fat consumption,30 and also lowered children’s body mass index (BMI), which persisted for years post-intervention.26 The benefits of existing school-based interventions may be enhanced by expanding the reach of initiatives in these programs. The U.S. Department of Agriculture’s Community Eligibility Provision enables children in high-poverty areas to receive school meals at no cost and without households having to apply.31 Serving food to children from low-income households reduces their risk of food insecurity and the financial burden on parents to provide meals. Further, including breakfast in school-provided meals may reduce parental strain and ensure that children do not skip breakfast, which is common among low-income children regardless of their food-security status.32 School boards in major U.S. cities have adopted programs to offer universal free breakfast in the classroom, which reduces some of the challenges associated with serving breakfast before school.33 Further, the Biden administration extended universal free lunch meals through the 2022 school year.34 Introducing universal school breakfast and lunch meals provides a sense of equality among children and reduces the stigma that “only poor students” participate in school meal programs.32,33
Some schools currently have such programs, inviting family members or caregivers to have breakfast with students in the school, laying the foundation for expanding the school breakfast program to include free meals for caregivers.35 Implementing an expanded school breakfast program in schools in low-income communities and inviting parents or caregivers to have breakfast with their children in school at least once a week may effectively increase family mealtimes among low-income households. Eating breakfast has positive health benefits;36 allowing parents to join the school breakfasts and making it a family meal may further increase the health of all household members. Additionally, school breakfasts may benefit families from low-income households by reducing food and grocery budgets and avoiding the skipping of breakfast. This programmatic strategy may address the cost burden of providing breakfast at home, and it also incorporates parents into a child-focused nutrition and obesity intervention.
Public school enrollment begins at kindergarten, leaving crucial years of child development unsupported by school-based programs. Extending the school-based family breakfast program to child care centers might be effective in reducing early childhood obesity. Existing infrastructure developed for the Child and Adult Care Food Program (CACFP)37 may be built on to develop a child care initiative that offers breakfast to parents and children before kindergarten. The CACFP is a federally funded program offering nutritious meals for children and adults enrolled in CACFP-affiliated care centers and provides meal reimbursement for low-income areas. The CACFP program can potentially reduce obesity at an early age and foster the integration of family breakfasts into daily routines for parents and children.
Opportunities in the Workplace
A significant portion of adult life is spent at the workplace, and as a result, this environment has great potential to influence individuals’ health. The World Health Organization identified the workplace as an influential environment for offering health-promoting initiatives, including those regarding nutrition and physical activity.38 Low-wage and low-income workers face particular challenges at work and home, including limited time and resources. Therefore, workplace programs designed for low-income workers, such as the ones briefly described in the following paragraphs, attempt to address the challenges that workers face in balancing work and family demands and in meeting their health needs.
The Expanded Food and Nutrition Education Program (EFNEP), founded by the U.S. Department of Agriculture, specifically assists families from low-income households with “food and physical activity behaviors.”39 The core areas of this educational program are diet quality and physical activity. The EFNEP also implements strategies to include family members in health behavior education, which is strongly associated with positive and robust health behavior changes in children. To improve access to this program, EFNEP services could be offered at the workplace. If employers partnered with EFNEP coordinators to conduct educational sessions for employees, and potentially their families, employees who are caregivers would receive the necessary education to promote healthy habits in their households. Overall, the EFNEP is an incredibly valuable tool for promoting health and reducing obesity among children. Expanding the program to the workplace would make EFNEP much more accessible to the families it works to assist.
In addition, workplace wellness programs (WWPs) provide a platform of established practices and initiatives for extending obesity interventions to children of employees. These initiatives are well established within the United States; as of 2020, 53% of small companies (i.e., <200 employees) and 81% of large companies implemented a wellness program.40 Advantages of these programs include that they are widely used, range in implementation strategy and topic, and show robust health and behavior improvements, including increased physical activity, increased fruit and vegetable consumption, decreased fat intake, and reduced weight and/or body mass index.41,42 WWPs can be used to encourage physical activity in children and promote family meals. This is especially important during the summer where prior research has indicated that low-income children experienced weight gain over the summer compared to the school year.43 WWP program extensions might include inviting families to engage in corporate-sponsored fitness initiatives or workplace-hosted family meals. Extending WWPs to include employees’ children may result in better child nutrition and physical activity. An additional advantage of using the workplace to address childhood obesity is that this strategy incorporates parents into the intervention, a successful component of FBT.21,22 Thus, the workplace can be influential in addressing the childhood obesity epidemic.
The workplace may also be a site to establish healthier food behaviors for workers from low-income households, such as promoting family meals at work. Inviting children into the workplace for the summer months provides a place for families to eat together. There are existing initiatives, such as the Summer Food Service Program (SFSP), providing healthy food to children and teens in low-income areas during the summer. However, participation in the SFSP is low (about 16% of eligible children participate).44 Reallocating some resources used in the SFSP to serve low-income families in the workplace could increase participation by providing children food in the same place as their parent’s work. This option will provide an opportunity for families from low-income households to eat together and reduce the strain of squeezing in meals at home before or after work. However, for successful implementation of such programs, challenges would first need to be addressed such as transportation for children to and from the workplace, staff and infrastructure for serving meals, and child care at the workplace. Employers may have to work with individuals or organizations who volunteer to assist with such programs.
In addition, WWPs offer an efficient and effective means of delivering and evaluating programs that promote physical activity among employees and that offer opportunities to reach socially disadvantaged groups.45 The 2016 National Physical Activity Plan provides a thorough foundation for companies to launch individual WWPs.46 Employer-sponsored physical activity opportunities can encourage parents to be more physically active and consequently enable children to be physically active; as a result, this increases children’s calorie expenditure through parental modeling and counters the rise of childhood obesity. However, such programs must be adapted to be implemented in work settings in order to address barriers preventing physical activity (e.g., air pollution, less access to recreation facilities, public and infrastructure safety issues).45
Challenges and Considerations
It is important to recognize that in many family-based interventions, the programs include only mothers, and that research including fathers, families from low-income households, and immigrant families is limited.47,48 The strategic principles established in most family-based research, often with majority White families, are applied here with a lens to a different demographic, and that may require alterations to elicit equivalent or more promising results.
While there are challenges to implementing WWPs, workplace efforts focused on reducing childhood obesity do not need to be a one-size fits all approach. For instance, prior research has indicated that children experience weight gain over the summer compared to the school year.43 Yet, workplace efforts to reduce childhood obesity need not be implemented only over the summer to compensate for the lack of school-based scheduling. Providing year-round efforts in the workplace to address childhood obesity is an important consideration. Additionally, workplace-sponsored physical activity need not occur only in the workplace or even require child care services. For example, businesses might encourage physical activity by reimbursing or subsidizing enrollment fees or monthly dues associated with gym or fitness studio memberships, or extending “steps-per-day” challenges and prizes to the children of employees.
A large challenge in the workplace is developing strategies to motivate employers to expand services to employees from low-income households and their families. However, many companies have been expanding their WWPs in recent years despite potentially discouraging obstacles.41 The widespread implementation of WWPs is, in part, due to flexible implementation strategies that can be tailored to the needs of individual employers, including those that may be hesitant to expand such programs.42 In 2017, about 70% of surveyed companies provided wellness resources and information: 30% of companies provided weight-loss programs, 16% provided nutritional counseling, and between 8% and 26% offered physical activity or fitness-related benefits.49 Another example is an intervention delivering fresh fruit at work, designed to reach low-wage employees; it was successful in improving families’ fruit and vegetable consumption and their purchasing of fruits and vegetables.50 Therefore, it is not unrealistic to recommend the expansion of WWPs as a strategy to help reduce child obesity. Moreover, WWPs can offer a large return on investment—investing in WWPs has been shown to reduce health care costs and absenteeism and to increase workforce productivity51—especially given the low costs of implementation.42 Implementing WWPs in workplace settings that employ people from low-income households will promote the health of those who are often also at risk of developing health issues and thus raising health care costs for both the employer and individual. Further, workforce wellness is often used as a measure of corporate success, so assisting with improving the health of employees could potentially increase corporate rankings.42 The multitude of motivating factors for implementing WWPs confirms that initiatives designed to increase access to these programs for families, particularly employees from low-income households, can have great potential.
Conclusion
Researchers and professionals working to eliminate childhood obesity specifically among low-income populations have numerous opportunities to influence policies pertaining to improving children’s and families’ dietary behaviors and physical activity. Given the severity of childhood obesity as a public health problem, with large disparities that vary across race, ethnicity, and income, the strategies discussed in this brief would especially benefit low-income and racially and ethnically minoritized children and families. Further, the strategies are beneficial to any child or family struggling with nutrition and physical activity, regardless of racial or ethnic minoritized status or income. Family-based interventions in schools, child care centers, and workplaces call for a simple refocusing of current policy and program infrastructure in order to make feasible the expansion of such programs.
Recommendations for Practitioners, Scholars, and Policymakers
- Provide opportunities for parents to participate in school-provided breakfast and lunch meals.
- Extend workplace wellness programs to improve child and family physical activity.
- Increase the prevalence of family meals by redirecting resources from existing federally funded programs such as the Summer Food Service Program.
- Encourage family-based research in nontraditional family settings, such as schools and workplaces, to evaluate nutrition and physical activities policies that are designed to address childhood obesity.
Author Bios
Daphne C. Hernandez is an Associate Professor and Lee and Joseph Jamail Distinguished Professor at the University of Texas Health Science Center at Houston’s Cizik School of Nursing. Her work focuses on food insecurity, stress, and health among vulnerable populations, including Hispanic immigrants.
Kendall R. Brice graduated with an undergraduate degree in kinesiology from Rice University. She is currently working on her Master’s of Science in prosthetics and orthotics at Baylor College of Medicine. She has found nutrition to be a common intersection of her interests in athletics, kinesiology, agriculture, and orthotics and prosthetics.
Jerica M. Berge is a Professor and Vice Chair for Research in the Department of Family Medicine and Community Health at the University of Minnesota Medical School. She is both a behavioral health clinician and a researcher. She is also the director of the Healthy Eating and Activity Across the Lifespan Center.
References
1. Sahoo, K., Sahoo, B., Choudhury, A. K., Sofi, N. Y., Kumar, R., & Bhadoria, A. S. (2015). Childhood obesity: Causes and consequences. Journal of Family Medicine and Primary Care, 4(2), 187–192. https://doi.org/10.4103/2249-4863.154628
2. Thorpe, K. E., Florence, C. S., Howard, D. H., & Joski, P. (2004). The impact of obesity on rising medical spending. Health Affairs, 23(Suppl. 1), W4-480–W4-486. https://doi.org/10.1377/hlthaff.W4.480
3. Wang, Y., Beydoun, M. A., Liang, L., Caballero, B., & Kumanyika, S. K. (2008). Will all Americans become overweight or obese? Estimating the progression and cost of the U.S. obesity epidemic. Obesity, 16(10), 2323–2330. https://doi.org/10.1038/oby.2008.351
4. Wang, Y., & Beydoun, M. A. (2007). The obesity epidemic in the United States—gender, age, socioeconomic, racial/ethnic, and geographic characteristics: A systematic review and meta-regression analysis. Epidemiologic Reviews, 29(1), 6–28. https://doi.org/10.1093/epirev/mxm007
5. Fryar, C. D., Carroll, M. D., & Afful, J. (2020). Prevalence of overweight, obesity, and severe obesity among children and adolescents aged 2–19 years: United States, 1963–1965 through 2017–2018. www.cdc.gov/nchs/data/hestat/obesity-child-17-18/obesity-child.htm
6. Ogden, C. L., Carroll, M. D., Fakhouri, T. H., Hales, C. M., Fryar, C. D., Li, X., & Freedman, D. S. (2018). Prevalence of obesity among youths by household income and education level of head of household—United States 2011–2014. MMWR: Morbidity and Mortality Weekly Report, 67(6), 186–189. https://doi.org/10.15585/mmwr.mm6706a3
7. Singh, G. K., Siahpush, M., & Kogan, M. D. (2010). Rising social inequalities in U.S. childhood obesity, 2003–2007. Annals of Epidemiology, 20(1), 40–52. https://doi.org/10.1016/j.annepidem.2009.09.008
8. Andrea, S. B., Hooker, E. R., Messer, L. C., Tandy, T., & Boone-Heinonen, J. (2017). Does the association between early life growth and later obesity differ by race/ethnicity or socioeconomic status? A systematic review. Annals of Epidemiology, 27(9), 583–592. https://doi.org/10.1016/j.annepidem.2017.08.019
9. Roberto, C. A., Swinburn, B., Hawkes, C., Huang, T. T., Costa, S. A., Ashe, M., Zwicker, L., Cawley, J. H., & Brownell, K. D. (2015). Patchy progress on obesity prevention: Emerging examples, entrenched barriers, and new thinking. Lancet, 385(9985), 2400–2409. https://doi.org/10.1016/s0140-6736(14)61744-x
10. Sothern, M. S. (2004). Obesity prevention in children: physical activity and nutrition. Nutrition, 20(7), 704–708. https://doi.org/10.1016/j.nut.2004.04.007
11. Vandevijvere, S., Chow, C. C., Hall, K. D., Umali, E., & Swinburn, B. A. (2015). Increased food energy supply as a major driver of the obesity epidemic: A global analysis. Bulletin of the World Health Organization, 93(7), 446–456. https://doi.org/10.2471/BLT.14.150565
12. Berge, J. M., Truesdale, K. P., Sherwood, N. E., Mitchell, N., Heerman, W. J., Barkin, S., Matheson, D., Levers-Landis, C. E., & French, S. A. (2017). Beyond the dinner table: Who’s having breakfast, lunch and dinner family meals and which meals are associated with better diet quality and BMI in pre-school children? Public Health Nutrition, 20(18), 3275–3284. https://doi.org/10.1017/S1368980017002348
13. Neumark-Sztainer, D., Hannan, P. J., Story, M., Croll, J., & Perry, C. (2003). Family meal patterns: Associations with sociodemographic characteristics and improved dietary intake among adolescents. Journal of the American Dietetic Association, 103(3), 317–322. https://doi.org/10.1053/jada.2003.50048
14. Hammons, A. J., & Fiese, B. H. (2011). Is frequency of shared family meals related to the nutritional health of children and adolescents? Pediatrics, 127(6), e1565–e1574. https://doi.org/10.1542/peds.2010-1440
15. Berge, J. M., Wall, M., Hsueh, T.-F., Fulkerson, J. A., Larson, N., & Neumark-Sztainer, D. (2015). The protective role of family meals for youth obesity: 10-year longitudinal associations. Journal of Pediatrics, 166(2), 296–301. https://doi.org/10.1016/j.jpeds.2014.08.030
16. Berge, J. M., Rowley, S., Trofholz, A., Hanson, C., Rueter, M., MacLehose, R. F., & Neumark-Sztainer, D. (2014). Childhood obesity and interpersonal dynamics during family meals. Pediatrics, 134(5), 923–932. https://doi.org/10.1542/peds.2014-1936
17. Gunther, C., Rogers, C., Holloman, C., Hopkins, L. C., Anderson, S. E., Miller, C. K., Copeland, K. A., Dollahite, J. S., Pratt, K. J., Webster, A., Labyk, A. N., & Penicka, C. (2019). Child diet and health outcomes of the simple suppers program: A 10-week, 2-group quasi-experimental family meals trial. BMC Public Health, 19(1), Article 1657. https://doi.org/10.1186/s12889-019-7930-7
18. U.S. Department of Health and Human Services. (2018). Physical activity guidelines for Americans (2nd ed.). U.S. Department of Health and Human Services. https://health.gov/sites/default/files/2019-09/Physical_Activity_Guidel…
19. Brownson, R. C., Chriqui, J. F., Burgeson, C. R., Fisher, M. C., & Ness, R. B. (2010). Translating epidemiology into policy to prevent childhood obesity: The case for promoting physical activity in school settings. Annals of Epidemiology, 20(6), 436–444. https://doi.org/10.1016/j.annepidem.2010.03.001
20. Armstrong, S., Wong, C. A., Perrin, E., Page, S., Sibley, L., & Skinner, A. (2018). Association of physical activity with income, race/ethnicity, and sex among adolescents and young adults in the United States: Findings from the National Health and Nutrition Examination Survey, 2007–2016. JAMA Pediatrics, 172(8), 732–740. https://doi.org/10.1001/jamapediatrics.2018.1273
21. Wilfley, D. E., Staiano, A. E., Altman, M., Lindros, J., Lima, A., Hassink, S. G., Dietz, W. H., Cook, S., & The Improving Access Systems of Care for Evidence-Based Childhood Obesity Treatment Conference Workgroup. (2017). Improving access and systems of care for evidence-based childhood obesity treatment: Conference key findings and next steps. Obesity, 25(1), 16–29. https://doi.org/10.1002/oby.21712
22. Stice, E., Shaw, H., & Marti, C. N. (2006). A meta-analytic review of obesity prevention programs for children and adolescents: The skinny on interventions that work. Psychological Bulletin, 132(5), 667–691. https://doi.org/10.1037/0033-2909.132.5.667
23. Janicke, D. M., Steele, R. G., Gayes, L. A., Lim, C. S., Clifford, L. M., Schneider, E. M., Carmody, J. K., & Westen, S. (2014). Systematic review and meta-analysis of comprehensive behavioral family lifestyle interventions addressing pediatric obesity. Journal of Pediatric Psychology, 39(8), 809–825. https://doi.org/10.1093/jpepsy/jsu023
24. Skelton, J. A., & Beech, B. M. (2011). Attrition in pediatric weight management: A review of the literature and new directions. Obesity Reviews, 12(5), e273–281. https://doi.org/10.1111/j.1467-789X.2010.00803.x
25. Stokes, N., Spruance, L., Patten, E. V., & Lybbert, E. K. (2019). Teachers’ experience and perspectives of traditional breakfast and breakfast in the classroom. Journal of Nutrition Education and Behavior, 51(8), 936–945. https://doi.org/10.1016/j.jneb.2019.04.004
26. Taylor, R. W., McAuley, K. A., Barbezat, W., Farmer, V. L., Williams, S. M., & Mann, J. I. (2008). Two-year follow-up of an obesity prevention initiative in children: The APPLE project. American Journal of Clinical Nutrition, 88(5), 1371–1377. https://doi.org/10.3945/ajcn.2007.25749
27. Johnson, D. B., Podrabsky, M., Rocha, A., & Otten, J. J. (2016). Effect of the healthy hunger-free kids act on the nutritional quality of meals selected by students and school lunch participation rates JAMA Pediatrics, 170(1), Article 153918. https://doi.org/10.1001/jamapediatrics.2015.3918
28. Louie, D., Sanchez, E. J., Faircloth, S., & Dietz, W. A. (2003). School-based policies: Nutrition and physical activity. Journal of Law, Medicine & Ethics, 31(4), 73–75. https://doi.org/10.1111/j.1748-720x.2003.tb00759.x
29. USDA Food and Nutrition Service. (2013). National School Lunch Program and School Breakfast Program: Nutrition standards for all foods sold in school as required by the Healthy, Hunger-Free Kids Act of 2010—Interim final rule. Federal Register, 78(125), 39067–39120.
30. Jaime, P. C., & Lock, K. (2009). Do school based food and nutrition policies improve diet and reduce obesity? Preventive Medicine, 48(1), 45–53. https://doi.org/10.1016/j.ypmed.2008.10.018
31. U.S. Department of Agriculture Food and Nutrition Service. (2019, April 19). Community eligibility provision. www.fns.usda.gov/cn/community-eligibility-provision
32. Askelson, N. M., Golembiewski, E. H., Bobst, A., Delger, P. J., & Scheidel, C. A. (2017). Understanding perceptions of school administrators related to school breakfast in a low school breakfast participation state. Journal of School Health, 87(6), 427–434. https://doi.org/10.1111/josh.12511
33. Bernstein, L. S., McLaughlin, J. E., Crepinsek, M. K., & Daft, L. M. (2004). Evaluation of the School Breakfast Program Pilot Project: Final report. (Report No. CN-04-SBP, Project Officer: Anita Singh). U.S. Department of Agriculture, Food and Nutrition Service, Office of Analysis, Nutrition, and Evaluation, Alexandra, VA. https://files.eric.ed.gov/fulltext/ED486532.pdf
34. U.S. Department of Agriculture. (2021, April 20). USDA issues pandemic flexibilities for schools and day care facilities through June 2022 to support safe
reopening and healthy, nutritious meals. www.usda.gov/media/press-releases/
2021/04/20/usda-issues-pandemic-flexibilities-schools-and-day-care-facilities
35. Marshall Elementary School. (2018). Marshall Elementary School breakfast buddies. https://marshallpfa.membershiptoolkit.com/home
36. Lien, L. (2007). Is breakfast consumption related to mental distress and academic performance in adolescents? Public Health Nutrition, 10(4), 422–428. https://doi.org/10.1017/S1368980007258550
37. Larson, N., Ward, D. S., Neelon, S. B., & Story, M. (2011). What role can child-care settings play in obesity prevention? A review of the evidence and call for research efforts. Journal of the American Dietetic Association, 111(9), 1343–1362. https://doi.org/10.1016/j.jada.2011.06.007
38. World Health Organization. (2013). Global action plan for the prevention and control of noncommunicable diseases 2013–2020. https://apps.who.int/iris/bitstream/handle/10665/94384/9789241506236_en…
39. U.S. Department of Agriculture. (2017). The Expanded Food and Nutrition Education Program policies. National Institute of Food and Agriculture. https://nifa.usda.gov/sites/default/files/program/EFNEP-Policy-December…
40. Aldana, S. (2022, August 1). 5 workplace wellness statistics every employer should know 2022 updated. WellSteps. www.wellsteps.com/blog/2020/01/02/workplace-wellness-statistics-wellnes…
41. Mattke, S., Liu, H., Caloyeras, J., Huang, C. Y., Van Busum, K. R., Khodyakov, D., & Shier, V. (2013). Workplace wellness programs study: Final report. www.rand.org/pubs/research_reports/RR254.html
42. Wipfli, H., Zacharias, K. D., Hundal, N., Shigematsu, L. M. R., Bahl, D., Arora, M., Bassi, S., & Kumar, S. (2018). Workplace wellness programming in low-and middle-income countries: A qualitative study of corporate key informants in Mexico and India. Globalization and Health, 14(1), Article 46. https://doi.org/10.1186/s12992-018-0362-9
43. Reesor, L., Moreno, J. P., Johnston, C. A., & Hernandez, D. C. (2019). School‐based weight management program curbs summer weight gain among low‐income Hispanic middle school students. Journal of School Health, 89(1), 59–67. https://doi.org/10.1111/josh.12713
44. U.S. Department of Agriculture Food and Nutrition Service. (2014). Food that’s in when school is out—The Summer Food Service Program and afterschool meals. www.fns.usda.gov/sfsp/food-thats-when-school-out-summer-food-service-pr…
45. Tabak, R. G., Strickland, J. R., Stein, R. I., Dart, H., Colditz, G. A., Kirk, B., Dale, A. M., & Evanoff, B. A. (2018). Development of a scalable weight loss intervention for low-income workers through adaptation of interactive obesity treatment approach (iOTA). BMC Public Health, 18(1), Article 1265. https://doi.org/10.1186/s12889-018-6176-0
46. Physical Activity Alliance. (2020). National physical activity plan. https://paamovewithus.org/wp-content/uploads/2020/07/National-PA-Plan.p…
47. Davison, K. K., Kitos, N., Aftosmes-Tobio, A., Ash, T., Agaronov, A., Sepulveda, M., & Haines, J. (2018). The forgotten parent: Fathers’ representation in family interventions to prevent childhood obesity. Preventive Medicine, 111, 170–176. https://doi.org/10.1016/j.ypmed.2018.02.029
48. Gicevic, S., Aftosmes-Tobio, A., Manganello, J. A., Ganter, C., Simon, C. L., Newlan, S., & Davison, K. K. (2016). Parenting and childhood obesity research: A quantitative content analysis of published research 2009–2015. Obesity Reviews, 17(8), 724–734. https://doi.org/10.1111/obr.12416
49. Society for Human Resource Management. (2017). 2017 employee benefits: Remaining competitive in a challenging talent marketplace. www.shrm.org/hr-today/trends-and-forecasting/research-and-surveys/Docum…
50. Backman, D., Gonzaga, G., Sugerman, S., Francis, D., & Cook, S. (2011). Effect of fresh fruit availability at worksites on the fruit and vegetable consumption of low-wage employees. Journal of Nutrition Education and Behavior, 43(4, Suppl. 2), S113–S121. https://doi.org/10.1016/j.jneb.2011.04.003
51. Baicker, K., Cutler, D., & Song, Z. (2010). Workplace wellness programs can generate savings. Health Affairs, 29(2), 304–311. https://doi.org/10.1377/hlthaff.2009.0626
Copyright © 2022 National Council on Family Relations
This policy brief may be duplicated, distributed, or posted electronically with attribution to the National Council on Family Relations.
Inclusion of portions or all of this brief in printed or electronic textbooks, anthologies, or other publications requires permission from NCFR.
The views expressed within this publication may not represent the views or policies of the entire organization.
To see all NCFR research briefs and policy briefs, visit ncfr.org/resources/research-and-policy-briefs
Elaine A. Anderson, Policy Brief Editor